WITH an increasing number of gluten-free products appearing on supermarket shelves, celebrity chefs bringing out gluten-free cookbooks and trendy restaurants offering gluten-free menu choices, avoiding or restricting foods that contain gluten may well seem to be the new healthy eating trend. But is it really healthier or only for people with a diagnosed medical condition?
Of course, there may be a few people who see it as a fashion choice, but most people wouldn't choose to cut out such a large part of a conventional modern diet without good reason to.
What is gluten?
Gluten is a protein complex found in wheat, barley and rye and any foods containing them. Because most oats are processed in factories that also process wheat, they are usually 'contaminated' with wheat (flour gets everywhere!) unless specifically labelled 'gluten-free'. However, some people who react to gluten also react to 'gluten-free' oats.
Gluten is what gives bread its bounce: its gluey structure helps to trap air to give an appealing sponginess. In fact, most of the bread we eat today uses wheat that has been bred (no pun intended!) to have a much higher gluten content than traditional varieties, such as spelt, for precisely this reason.
Is avoiding gluten just another food fad for attention seekers and fussy eaters?
Well, no, I don't think so. Of course, there may be a few people who see it as a fashion choice, but most people wouldn't choose to cut out such a large part of a conventional modern diet without good reason to. There are two specific conditions that require complete and permanent avoidance of all gluten grains and foods containing them:
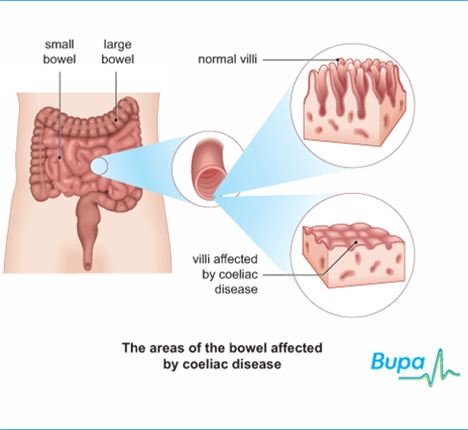
Coeliac Disease
Coeliac Disease is caused by an auto-immune reaction to gluten, triggering damage to the lining of the small intestine and leading to issues with absorption of nutrients such as anaemia and osteoporosis. It may also be linked to other health issues and, given the involvement of the digestive system, may be initially mistaken for IBS (irritable bowel syndrome).
Once believed to be a rare condition, Coeliac UK, the charity that supports sufferers, states that 1 in 100 people have coeliac disease but that it’s woefully under-diagnosed, estimating that only 10-15 per cent of sufferers have a formal diagnosis.
Coeliac disease is diagnosed via a blood test and a gut biopsy and you must be eating gluten foods for the test to be valid. There is a high frequency of falsely negative results from the blood tests.
Gluten Sensitivity
 Gluten sensitivity refers to an auto-immune reaction to gluten which may or may not involve the small intestine. A greater awareness of this condition, sometimes referred to as non-coeliac gluten sensitivity, has taken place even within the last six months with articles on the subject appearing in publications such as the prestigious British Medical Journal.
Gluten sensitivity refers to an auto-immune reaction to gluten which may or may not involve the small intestine. A greater awareness of this condition, sometimes referred to as non-coeliac gluten sensitivity, has taken place even within the last six months with articles on the subject appearing in publications such as the prestigious British Medical Journal.
With gluten sensitivity you may have digestive symptoms (but test negative for coeliac disease) or you may have no digestive symptoms at all. Gluten sensitivity has been linked to numerous auto-immune conditions with some experts suggesting that all auto-immune diseases may be linked to gluten sensitivity. Symptoms can include IBS-type symptoms, fatigue, 'foggy' mind, joint pain, headaches, skin rashes, etc with some people having lots of symptoms and others only one or two.
At the moment, the only way to identify gluten sensitivity is by eliminating gluten from the diet (this should only be done with support from a health professional) and monitoring symptoms. There are tests available in the USA which test for a wider range of gluten-sensitivity markers than the current tests for coeliac disease but these are not yet available in the UK (anticipated later this year). Several of my clients have had negative tests for coeliac disease but know that eating gluten foods makes them very unwell.
What should I do if I think that I react to gluten?
Firstly, go and see your GP and ask to be tested for coeliac disease. Don't cut gluten out of your diet at this stage because the test measures antibodies to gluten which may not be present if you are not eating gluten grains.
If you have had a negative result from a test for coeliac disease but still suspect gluten to be a problem, I recommend you consult with a BANT-registered nutritional therapist (www.bant.org.uk for a practitioner listing) who can advise you. Gluten sensitivity runs in families so if another family member has coeliac disease, the likelihood of your having gluten sensitivity is increased.
The advice given here is not intended to replace medical advice. Always consult your GP if you are concerned about your health.
Clare Jones, BA(Hons), Dip ION, mBANT NTC & CNHC registered
Nutritional Therapy 07985 166606.
If you would like to make an appointment for a personal nutrition consultation with Clare, please contact her on the above number or visit Clare’s website: www.clarejones-nutrition.co.uk
Follow Clare on Twitter @ClareJonesNutri and Facebook www.facebook.com/ClareJonesNutritionalTherapy